What is hepatitis A?
Hepatitis A is a highly contagious and sometimes fatal liver disease. Historically, it was called infectious hepatitis. Today, the disease is more commonly known as hepatitis A, named after the virus that causes it. Each year, approximately 1.4 million people worldwide and 143,000 people in the United States become infected with hepatitis A, costing patients and employers millions of dollars in lost wages and lost productivity.
The incidence of hepatitis A varies throughout the world. Areas where hepatitis A is common or “endemic” are shown in the map below. In unprotected people traveling to highly endemic areas, hepatitis A occurs 10 to 100 times more frequently than typhoid fever and 1,000 times more often than cholera. Outbreaks of hepatitis A also occur in areas of low endemicity, including the United States.
| Worldwide prevalence of hepatitis A infection, 1995 |
| Adapted from the Centers for Disease Control and Prevention, August 199 |
How do people get hepatitis A?
|
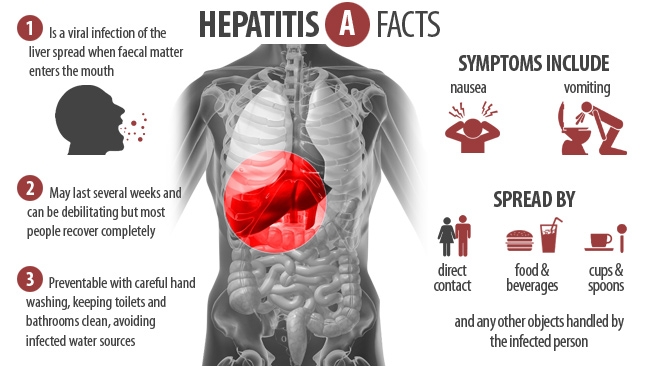
Hepatitis A is found in the stool of persons with hepatitis A. The virus is usually spread through person-to-person contact or through contaminated food and water. For example, you can get hepatitis A from an infected child if you don’t wash your hands after changing a diaper or from an infected person if they don’t wash their hands after going to the bathroom. If the fecal contaminant somehow gets on food – for example, if a contaminated cook handles food in a restaurant – the disease can spread quickly. |
|
|
A person can also get hepatitis A by drinking water that is contaminated with the virus or by eating food washed in contaminated water, such as raw or undercooked shellfish, salads, or unpeeled fruits. |
|
What are the symptoms of hepatitis A?
|
In those who develop symptomatic hepatitis A, flu-like symptoms, such as fever, chills, and a general feeling of weakness, may occur. Other symptoms may include anorexia, nausea, jaundice (yellowing of the eyes and skin), dark urine, light-colored stools, abdominal pain, and fatigue. Although hepatitis A does not result in chronic infection, complete recovery from hepatitis A can be slow. In children, especially in those younger than 6 years of age, there are often no symptoms. Adult patients with hepatitis A may be quite ill for at least a month, and full recovery can take up to 6 months. |
|
|
Up to 20% may have a relapse of the disease and may be impaired for as long as 15 months. In addition, it is estimated that 15% of patients require hospitalization for hepatitis A. |
|
Who is at increased risk of hepatitis A?
Children, teens, and adults who may be at high risk of hepatitis A or who could transmit the disease to others if they become infected include:
-
Persons traveling to areas of higher endemicity for hepatitis A. These areas include but are not limited to, Africa, Asia (except Japan), the Mediterranean basin, Eastern Europe, the Middle East, Central and South America, Mexico, and parts of the Caribbean
-
Persons living in or relocating to any community in the U.S. or abroad with one or more recorded hepatitis A outbreaks within the past 5 years
-
Military personnel
-
Persons who engage in high-risk sexual activity
-
Users of illicit injectable drugs
-
Hemophiliacs and other recipients of therapeutic blood products
-
Employees of day-care centers
-
Institutional care workers
-
Laboratory workers who handle live hepatitis A virus
-
Handlers of primate animals that may be harboring hepatitis A virus
Why is hepatitis A called a travel disease?
Hepatitis A is sometimes called a travel disease because it is the most frequently occurring, vaccine-preventable infection in travelers. Each year, approximately 24 million people from the United States visit, either on business or as tourists, areas where hepatitis A is endemic.
The incidence of hepatitis A disease in travelers increases with the length of travel and is highest for those who stay in or visit rural areas, trek in back country, or frequently eat or drink in areas with poor sanitary conditions. However, many travelers falsely assume that the risk of hepatitis A is present only under these conditions. In fact, hepatitis A can also occur among travelers who stay only in urban areas and luxury hotels.
Can I avoid hepatitis A if I don’t travel?
It is possible to become infected with hepatitis A virus without ever leaving the United States. Approximately 45% of the 34,243 cases reported in the United States from 1990-1992 occurred in people with no identifiable risk factors. For example, county-wide outbreaks have been occurring in Northern California since 1993. In Shasta County alone, more than 500 cases have occurred. Outbreaks of hepatitis A in the United States have also been associated with contaminated food, with infected foodhandlers, and with day-care centers. For example, in an outbreak in Memphis, Tennessee, more than 1,000 cases have been identified and authorities believe the virus is being spread by young children.
What steps can I take to help protect against hepatitis A?
Environmental Risks
There are things you can do to help protect yourself and others from the risk of hepatitis A.
Whether you are traveling to or living in areas where hepatitis A is endemic, or are at increased risk of contracting hepatitis A because of your work or lifestyle, most cases of hepatitis A can be avoided if you:
- Avoid untreated tap water in drinks or ice cubes. When drinking or brushing your teeth, use only bottled or boiled water.
- Do not eat unpeeled fruits, salads, uncooked vegetables, or raw shellfish (e.g., clams, oysters, and mussels). These foods can be contaminated with hepatitis A, even in “western” style restaurants and resorts.
- Do not eat food or drink beverages (except commercially bottled beverages) bought from street vendors.
Personal Actions
Since no specific medicine is available to treat hepatitis A once you are infected, it is very important to prevent the infection. One of the best ways to prevent the spread of hepatitis A is easy – proper hand washing.
Proper handwashing:
| 1. | Use warm water | 3. | Rub your soapy hands together for about 20 seconds | 5. | Turn off water with paper towel |
| 2. | Wet your hands before appyling | 4. | Rinse your hands thoroughly to remove all soap | 6. | Dry your hands with an air-dryer or a clean paper towel |
Prevent the spread with your own bare hands
Always wash your hands thoroughly after using the bathroom and make sure everyone in your family does too – especially children. Wash your hands just before eating or preparing food and immediately after touching anything that might contaminate your hands. If possible, in a day-care setting, wear disposable gloves when changing or handling the diaper of a child who may be infected.
Vaccination
Hepatitis A may also be avoided through vaccination with immune globulin (IG) – or hepatitis A vaccine.
IG contains antibodies (or protective proteins) to the hepatitis A virus. IG is relatively inexpensive and provides short-term protection against hepatitis A disease (generally 3 to 5 months).
Hepatitis A vaccines also help provide longer-term protection against hepatitis A. The total duration of protection is unknown at present, but in one study, protection was demonstrated for at least 4 years. Studies are ongoing. The vaccines contain a killed or inactivated virus that does not cause hepatitis A, but does stimulate the body’s immune system to make the antibodies that help protect against the virus.
Vaccines against hepatitis A are generally well tolerated. There may be pain, redness, tenderness, warmth, and irritation at the site where you receive the injection. Fever, abdominal pain, headache, fatigue, and allergic reactions may also occur.
Serious reactions are rare, but may occur. You should discuss potential side effects with your doctor.
As with all vaccines, vaccination with either IG or hepatitis A vaccine may not protect 100% of all those who are vaccinated.
Should I be vaccinated against hepatitis A?
Ask your doctor or travel medicine specialist whether you or your family members should be vaccinated against hepatitis A. If you plan to travel, ask them about vaccination at least 2 weeks before your departure. Be sure to discuss the benefits, as well as the risks, of vaccination against this disease.